UK Breastfeeding Trends
The World Breastfeeding Trends Initiative (WBTi) is a collaborative initiative to assess and monitor key breastfeeding policies and programmes (WBTi indicators), all drawn from the WHO Global Strategy and the Innocenti Declaration. It was launched by the International Baby Food Action Network (IBFAN) in 2004.
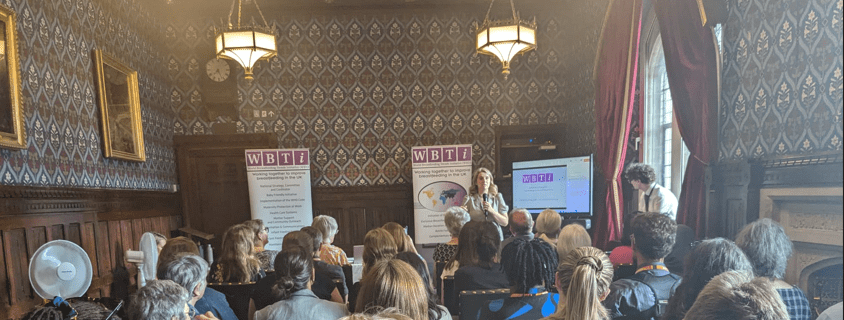
The first WBTi UK report (see media reports here) was launched in Parliament on 15 November 2016. The second report on the UK, covering 2023-24, was released in March 2015.
Currently over 100 countries are participating in the WBTi; the latest global report and details are available online, including the European 18-country report 2020.
Each report lists gaps and recommendations for each indicator to trigger actions that improve support for breastfeeding in that country.
Mothers and babies need the full network of support that is measured by the WBTi.
Follow the news and discussion on Twitter @wbtiUK and on our Facebook page.
Latest blogs
Sign up to our mailing list or volunteer
The WBTi UK Core Group for the 2016 Report
- Department of Health
- Public Health England
- Northern Ireland Regional Breastfeeding Lead
- Scotland Maternal and Infant Nutrition Coordinator
- Child and Maternal Health Observatory (ChiMat)
- National Infant Feeding Network (NIFN)
- Unicef UK Baby Friendly Initiative