Health professional training needs to include more on infant feeding
Gaps in health professional training on infant feeding have been one of the most talked-about findings of the WBTi project in the UK.
The soft launch of the second WBTi Report on UK infant feeding policies and programmes was held at Guy’s Hospital, London, on March 25th, with a focus on gaps in pre-registration training for health professionals.
The WBTi assessment also includes in-service training. In the UK, the main source is UNICEF Baby Friendly Initiative training.
What were the gaps?
Little has changed in these high level universal standards since the 2016 WBTi report. The most striking gap is that the general requirements for all nurses do not explicitly include infant feeding; this means that university health visitor training programs are not required to include much on breastfeeding, unless they are UNICEF Baby Friendly-accredited. Only 21% of university health visitor training programmes are BFI-accredited, although many health visitors will go on to receive in-service training as 69% of health visiting services in the community are now BFI- accredited. Nurses in other parts of the health system, from emergency rooms to oncology or women’s health, and even in paediatric and neonatal wards, have not routinely received training in breastfeeding.
Little support for hospitalised mothers
The WBTi team also conducted a survey of infant feeding leads on NHS Trust policies to support hospitalised mothers who are breastfeeding in wards other than maternity, for example to maintain their milk supply. We found that many Trusts lack such a policy. Scotland does have a guideline that has now been rolled out across the NHS in Scotland.
Sharing our findings
The event was well attended by key stakeholders, including representatives from the Department of Health and Social Care and devolved nations, health professional bodies, UNICEF Baby Friendly Initiative, and members of the WBTI Core Group.
Dr Bob Boyle of Imperial College set the scene with an historical background of infant feeding in the UK and globally. The WBTi team gave an overview of the report, emphasising the importance of every mother in the UK having access to an integrated network of infant feeding support, and the essential need for political commitment to enable this.
Mapping of pre-registration training standards against the WHO Education Checklist
The UK WBTI assessment maps national minimum standards for training on infant feeding topics against the Educational Checklist from WHO.
The WBTI mapping shows what any family, in any part of the UK, can expect as a minimum from their local health professionals, including not only midwives and health visitors, but also GPs, paediatricians, dietitians and pharmacists.
The assessment found some improvements, but many gaps remain, as can be seen in the chart below, with the red indicating the gaps. It is essential that everyone caring for parents have knowledge of breastfeeding. Health workers should be able to support parents’ goals, and avoid inadvertently undermining their infant feeding decisions.
WBTi summary table of breastfeeding topics in health professional standards
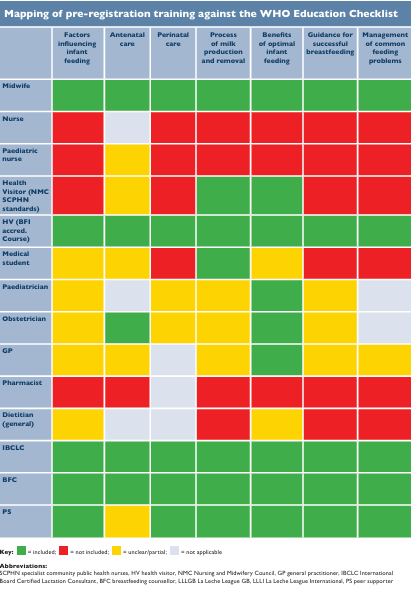
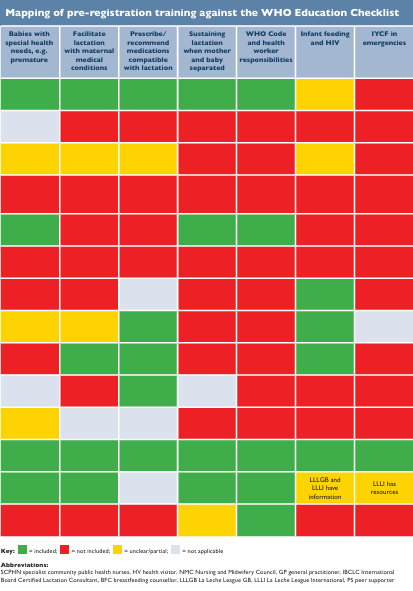
Table of basic standards in breastfeeding topics. More details can be found in Indicator 5 in the full report (Part 1). See Part 2 for a more detailed breakdown.
Author
Dr Alison Spiro is a member of the WBTi Steering Group. She is a retired NCT breastfeeding counsellor, specialist health visitor and hospital and community infant feeding lead, taking both trusts to Baby Friendly accreditation. She completed her MSc in 1994 and PhD in 2004 on Gujarati culture and breastfeeding, doing her fieldwork in Harrow and India.
Alison is the author of a book ‘Breastfeeding for Public Health, a guide for community health professionals’ published by Routledge.

