August 1-7th marks the World Breastfeeding Week. The theme is ‘Let’s make breastfeeding and work, work!’ The benefit of breastfeeding to health, the economy, work and the environment is widely documented. However, the UK remains one of the countries in the world with the lowest breastfeeding rate. Although 81% of mothers set out to breastfeed, only 1% of babies in the UK are still exclusively breastfed at 6 months. The question has always been why is breastfeeding rate so low in the UK?
Return to work is one of the key barriers to breastfeeding especially where the workplace is not breastfeeding friendly. A study published in 2007 by the Cohort Group found that mothers employed part-time or self-employed were more likely to breast-feed for at least 4 months than those employed full-time. The longer a mother delayed her return to work postpartum, the more likely she was to breast-feed for at least 4 months. Mothers were more likely to breastfeed for at least 4 months if their employer offered family-friendly or flexible work arrangements, or they received Statutory Maternity Pay plus additional pay during their maternity leave rather than Statutory Maternity Pay alone. This demonstrated that return to work could have a negative impact on breastfeeding if the mother is not properly supported.
Currently the UK does not have a legal framework that protects and promote breastfeeding in the workplace. The 1001 critical days strategy is there but does not have a legal backing to ensure that mothers are properly supported to continue breastfeeding should they choose to return to work early. A general assumption is made that mothers would take the full 52 weeks of maternity leave even though the leave is not properly paid. Mothers returning to work find it challenging to understand what they can and cannot do.
Though many employers are quick to showcase how family friendly they are in supporting working parents, breastfeeding remains an area in need of significant improvement. This is predominantly because the government has failed to recognise the benefits of breastfeeding and has failed to embed it in the current family friendly rights. Ideally, maternity leave should naturally go with a workplace breastfeeding policy. Other family friendly policies such as shared parental leave is not achieving its desired impact partly because of the lack of breastfeeding support in the workplace.
Mothers who intend to breastfeed for long may not share their maternity leave with their partners if support is not in place in the workplace.
These challenges were clearly articulates in the breastfeeding documentary titled ‘Breastfeeding: Not on the Agenda’which was followed by a call to action for the government to include breastfeeding in the family friendly rights to Make Breastfeeding and Work, Work.
NOTE from the WBTi team:
This petition incorporates many of the WBTi recommendations for action:
- Embed breastfeeding in the school curriculum and relevant health professionals training.
- See WBTi recommendations for Indicator 5 “Health Professional training” and our related blogs:
- Recommendations on health professional training: WBTi Report Part 1: indicator 5
- WBTi Report Part 2: Indicator 5 for details of each health profession’s training standards in infant and young child feeding
- WBTi blog on “What does your doctor know about breastfeeding? and our 2020 Eevent on “Doctors and Breastfeeding”
- Provide a policy on breastfeeding in the workplace which will protect the rights of breastfeeding mothers in the workplace.
- Our WBTi 2016 findings and recommendations on Indicator 4, maternity protection in the workplace
- Our other WBTi blogs on maternity protection and breastfeeding breaks in the workplace HERE and HERE
- Mandate all large public places like shopping malls, community centres, public libraries, museums, etc to provide breastfeeding rooms or spaces.
- Fully adopt The Code of Marketing of Breastmilk Substitutes to protect babies and their families from harmful commercial influences and undermining of breastfeeding for commercial profit; and to protect families who formula feed from the escalating costs of premium brands.
- Our WBTi 2016 findings and recommendations on Indicator 3: The International Code that the UK government implement the full Code and subsequent relevant WHA Resolutions in UK law and regulations, and also monitor and enforce these regulations.
- Further examples of Code violations in the UK in WBTi 2016 Report Part 2: Indicator 3
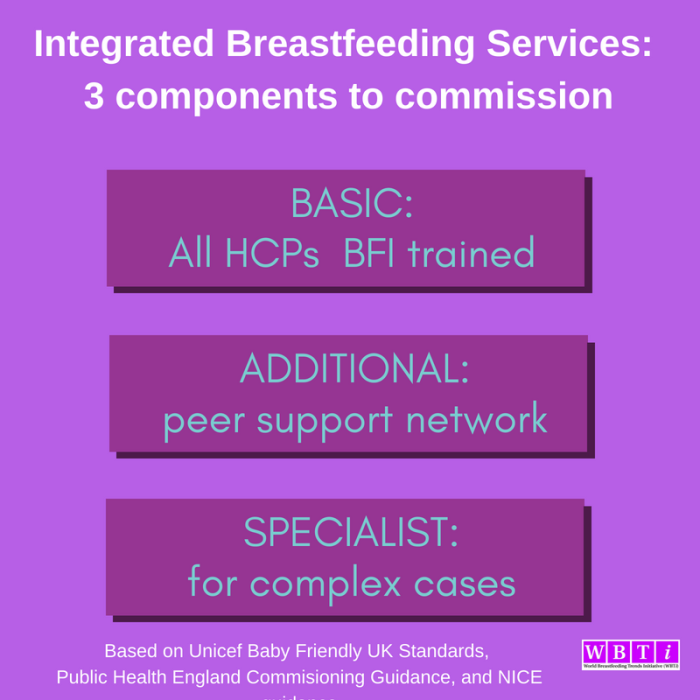
- Provide adequate 24/7 specialist lactation support in maternity services to actively counteract the culture of formula top-ups in hospitals; and to enable human donor milk to be more accessible as an option when mother’s milk is not immediately available.
- Guarantee a sustained funding support to breastfeeding organisations who play a key part in supporting mothers.
- Our WBTi 2016 findings and recommendations on Indicator 6: community-based support
- Additional findings in Part 2 including an audit of UK third sector breastfeeding support, and a list of cuts to community services
- Include breastfeeding support on the Net Zero Environmental Agenda.
Dr Ernestine Gheyoh Ndzi is the Associate Dean for Law and Police Studies at York St John University. Her research interest lies in Company Law and Employment Law. Ernestine has in the past four years been researching on shared parental leave and breastfeeding. Ernestine is a member of the Board of Trustees for The Breastfeeding Network. She is the producer of the breastfeeding documentary titled ‘Breastfeeding: Not on the Agenda. She is running a 9-webinar series exploring the benefits and challenges of breastfeeding. She is also leading on the campaign for change to support breastfeeding in the UK.