‘Breastfeeding: Not on the Agenda’ Webinar series: ‘Ready for Disaster? Infant and young child feeding in emergencies in the UK and Europe’ will be presented today by Helen Gray, WBTi Joint Coordinator.
NOTE: this presentation is now available on YouTube
This week’s topic in the “Breastfeeding: Not on the Agenda” series of webinars is the importance of planning for the protection of infant and young child feeding in emergencies, right here in the UK.
Infants, young children, pregnant and breastfeeding women are among the most vulnerable in any emergency situation, but they are almost invisible in our national resilience planning.
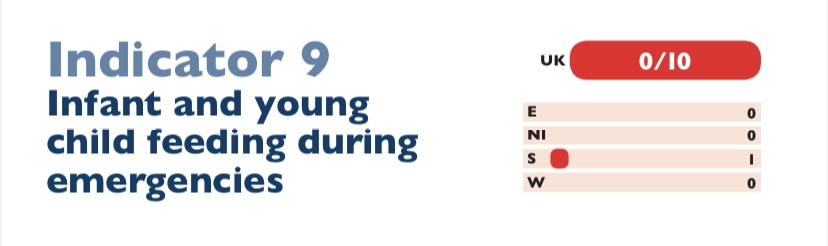
In the UK, the 2016 WBTi report found that while there is national guidance on the care of farm animals, pets, zoo animals and circus animals in emergencies, but there is no mention of infants or young children. There is an assumption that parents will take all responsibility for their own family – but too often there are no guidelines or recommendations to help them to prepare or handle an emergency.
Breastfeeding is a vital element in resilience and food security for families with infants: it provides immune protection and safe nutrition and fluids at any time, while providing both mother and child with comfort and resilience against stress. Skilled breastfeeding support is essential during emergencies, to enable breastfeeding dyads to continue.
In the UK, many infants are dependent on formula, which brings its own risks in an emergency. Infants who are not breastfed have reduced immunity to infections, in a situation where pathogens may be significantly increased due to contaminated water, or the crowding of evacuated families in rest centres. These infants depend on access to clean water, to a supply of suitable formula, and to hygienic preparation facilities and feeding equipment, and suitably trained support from responders and staff.
Local emergency planning in England and Wales is devolved to Local Resilience Forums (LRF). A recent study of LRF guidance for the public on emergency “grab bags,” by WBTi team member Patricia Wise, found that out of 42 LRF websites in England and Wales, only 27 even mention infant supplies, and 18 of those give only generic information rather than specific advice on what to pack for infants in an emergency. Northern Ireland included a generic ‘special equipment for children’ in its grab bag recommendations.
It is not difficult to include these supplies, facilities and training in every local resilience plan – there are resources and model operational guidance on the Infant Feeding in Emergencies Core Group website.
- Contact your Local Resilience Forum (LRF) and ask them what they include in their “grab-bag” lists and their planning for rest centres in case of evacuation.
The climate crisis is contributing to increased frequency and severity of natural disasters. The Australian Government recently funded a large research project, Babies and Young Children in the Black Summer (BiBS) Study, into the impact of the Black Summer Bushfires on families with infants and young children, conducted by the Australian Breastfeeding Association, Dr Michelle Hamrosi and Dr Karleen Gribble from Western Sydney University. One of the findings from this study was that parents with young children felt that they did not have the right information in time, that they needed extra preparation and extra time to evacuate. In fact, the title of the BiBS report is “Want to help the children? Help the parents.”
The recent global COVID-19 emergency also had a disproportionate impact on families with infants and young children. Despite consistent guidance from WHO emphasising the importance of breastfeeding to infant health, and supporting mothers to maintain breastfeeding or at least their milk supply if possible, many countries routinely separated mothers and newborns, despite disrupting breastfeeding with the risks that would entail to maternal and infant health and wellbeing (Vu et al. 2020).
In the UK, families are also experiencing long term crises of food insecurity, especially during the current cost of living crisis. UNICEF Baby Friendly UK, NIFN and First Steps Nutrition have produced important guidance for local authorities on how to support these families. First Steps Nutrition have produced several related reports on food security for families with infants and on the impact of the cost of living crisis.
ACTION! contact your local authority and ask them
- Whether they are implementing the UNICEF BFI guidance on food insecurity for families with infants
- Whether your Local Resilience Forum plan includes infants and young children
- Whether local guidance follows the Operational Guidance for Emergency Relief Staff and for Programme Managers
- Email us to tell us what you find out! wbti@ukbreastfeeding.org
- Volunteer to help with WBTi’s research on infant feeding in emergencies for our upcoming second assessment of UK policies!
- Ask your MP to ask questions about this in Parliament!
This webinar is part of the documentary and webinar series “Breastfeeding: Not on the Agenda” on breastfeeding, hosted by Dr Ernestine Ndzi from York St John University.
You can register for upcoming webinars here.
Previous webinars in the series and the documentary are available on YouTube.
Helen Gray is Joint Coordinator of the World Breastfeeding Trends Initiative (WBTi) project in the UK.
She is the Policy and Advocacy Lead for Lactation Consultants of Great Britain. She represents La Leche League of Great Britain on the UK Baby Feeding Law Group (BFLG), which works to bring the International Code of Marketing of Breastmilk Substitutes into UK law.
Helen’s background in anthropology and human evolution has influenced her interest in how breastfeeding, and the way we nurture our babies, are influenced by both human biology and culture.
Her current advocacy focus is the need for strong policies to protect infant feeding in emergencies. She has written several articles and chapters on the subject and served on the Advisory Panel for a London Food Resilience research project. She now represents BFLG on the global Infant Feeding in Emergencies Core Group.





































 Helen Gray MPhil IBCLC is Joint Coordinator of the World Breastfeeding Trends Initiative (WBTi) UK Working Group. She is on the national committee of Lactation Consultants of Great Britain, and is also an accredited La Leche League Leader. She is a founding member of National Maternity Voices. She represents LLLGB on the UK Baby Feeding Law Group, and serves on the La Leche League International special committee on the International Code.
Helen Gray MPhil IBCLC is Joint Coordinator of the World Breastfeeding Trends Initiative (WBTi) UK Working Group. She is on the national committee of Lactation Consultants of Great Britain, and is also an accredited La Leche League Leader. She is a founding member of National Maternity Voices. She represents LLLGB on the UK Baby Feeding Law Group, and serves on the La Leche League International special committee on the International Code.

